Gluten, Autoimmunity and Leaky Gut Syndrome
 I highly recommend reading Chris Kresser’s blog if you are interested in autoimmune disease, celiac disease, digestive health and leaky gut syndrome. Most recently, he interviewed Dr. Alessio Fasano, a pioneer in the field of gut and autoimmune disease. He is a world-renown pediatric gastroenterologist, and the researcher who published the groundbreaking study in the Annals of Medicine that established the prevalence of Celiac disease–1 in 133 people in the U.S.–nearly 100 times greater than the previous estimate. He also helped discover the ancient molecule, zonulin, which regulates intestinal permeability in the digestive tract and is a major component of leaky gut syndrome. Dr. Fasano has been featured in hundreds of interviews and media outlets such as The Wall Street Journal, NPR, The New York Times Magazine, National Geographic, USA Today, the LA Times, Good Morning America.
I highly recommend reading Chris Kresser’s blog if you are interested in autoimmune disease, celiac disease, digestive health and leaky gut syndrome. Most recently, he interviewed Dr. Alessio Fasano, a pioneer in the field of gut and autoimmune disease. He is a world-renown pediatric gastroenterologist, and the researcher who published the groundbreaking study in the Annals of Medicine that established the prevalence of Celiac disease–1 in 133 people in the U.S.–nearly 100 times greater than the previous estimate. He also helped discover the ancient molecule, zonulin, which regulates intestinal permeability in the digestive tract and is a major component of leaky gut syndrome. Dr. Fasano has been featured in hundreds of interviews and media outlets such as The Wall Street Journal, NPR, The New York Times Magazine, National Geographic, USA Today, the LA Times, Good Morning America.
Here are some fascinating tid-bits from this interview.
An Autoimmune Disease With A Known Cure
Celiac disease is the only autoimmune disease where we actually know the environmental trigger. In other words, we know the cure for this disease–avoidance of gluten. With other autoimmune conditions, the environmental trigger could be multiple things–infectious agents like molds, bacteria, yeast, heavy metals, food allergens, or other antigens in the environment that trigger the immune system to start attacking itself.
According to Dr. Fasano, “We don’t know what makes people sick with diabetes or MS, but (with celiac disease) it’s indisputable gluten, this strange protein contained in many grains, including wheat, rye, and barley, to be the culprit that leads to autoimmunity on that specific genetic background. That implies that celiac disease is the only autoimmune disease for which we have a treatment.”
Celiac Understood during World War II
Celiac disease was described for centuries. A pediatric gastroenterologist named Dicke from the Netherlands observed that during World War II, mortality from celiac disease (you could die from celiac disease at that time) dropped by 35-40%. When the war was over, mortality rates went back up to pre-war status. The correlation he discovered was that during the war wheat was not available. Flour was made with potato starch. The unavailability of gluten-containing grains during the war was the main parallel that coincided with lowered mortality. When the war ended, gluten became available again and disease returned.
3 Factors That Cause Autoimmune Disease
Autoimmune disease comes about by having 3 factors, according to Dr. Fasano. First, you must have the genetic predisposition for being susceptible to an autoimmune disease. Second, the body must be exposed to an environmental factor that will trigger the immune system to respond. Third, a person with an autoimmune disease must have some degree of compromised mucosal barriers in the digestive tract which allows the environmental trigger to reach the body’s the immune system. This is often referred to as “leaky gut syndrome.”
Zonulin, Intestinal Permeability and Autoimmune Disease
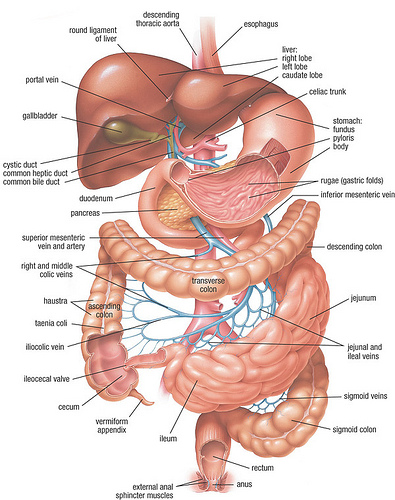
When we think about the intestine, most of us imagine a long tube from mouth to anus. What we don’t often think about is that the cells in the intestinal wall have doors or channels in between them. These doors can open and close. Dr. Fasano made the discovery that a molecule called zonulin is responsible for signaling the opening and closing of these doors in the intestine. When a person with celiac disease consumes gluten, a ton of zonulin gets produced, opening the doors in the intestine wall and allowing larger proteins such as gluten and other particles to enter the blood stream. The immune system in the blood stream becomes overwhelmed and creates an autoimmune response. Dr. Fasano explains the process below:
“What is the difference between everybody and the people that develop a problem with gluten like celiac disease is that while for me, for example, because I don’t have a problem. I eat a Big Mac. I have gluten in there. These fragments release zonulin, which increases permeability. Stuff comes through, including gluten. My immune system that is tuned to do the job right will clean up the mess, and I will not even know that all that happened. Also because this open-and-close is short. It’s a matter of minutes that it will open and a matter of minutes that will turn to be closed. People with celiac disease, on the other hand, when they do something like that, not only do they have much more zonulin produced than I do, but also the opening is much more prolonged because these doors get stuck open, and therefore you give much more time for substances from the environment, including gluten, to come through. And now on this other side, you find this immune system that is not tuned to do the job right, and when they see this enemy, they start to mount an immune response to attack your own body, and that leads to celiac disease.”
For people with celiac disease, avoiding gluten improves their health. However, even on a gluten-free diet, people with celiac disease are still prone to having larger amounts of zonulin in their body. In fact, this is also true for people with other autoimmune diseases.
“We have seen this in celiac disease and type 1 diabetes and multiple sclerosis. It has been proven in Crohn’s disease and in another category there are tumors ovarian cancer, pancreatic cancer, glioma, these kinds of cancers, and then in diseases of the nervous system, including schizophrenia and autism,” said Fasano.
Gluten Sensitivity
Testing negative for celiac disease does not mean that you are safe to eat gluten. Some people have what is called gluten sensitivity which involves an immune response to gluten but on a smaller scale. Dr. Fasano states:
“We started to dig into this situation a little bit more, and sure enough, we discovered that there is another form of gluten reaction that we don’t call gluten intolerance anymore because we went through a revision of nomenclature, but we call it gluten sensitivity. And it turns out to be an immune response to gluten not on an autoimmune basis like in celiac disease, not even on an allergic basis because we know that sometimes wheat can induce an allergic reaction like any other foodstuff. They probably experience what everybody does, so a transient increase in permeability but long enough to allow gluten to come through and be seen by the immune system that will generate an inflammatory response that’s not as severe as the one that’s typical of celiac disease.”
To read more of Chris Kresser’s interview of Dr. Fasano, check out: RHR: Pioneering Researcher Alessio Fasano M.D. on Gluten, Autoimmunity and Leaky Gut.