Spotlight on Your Bones: Part II
Dr. Holly Castle Discusses A Whole-Person Approach to Preventing Osteoporosis
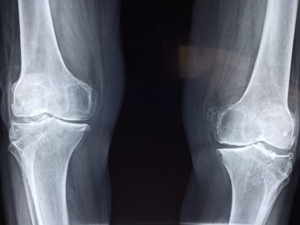
As much as we strive to eat a healthy diet, get 8 hours of sleep each night, exercise, and manage our stress, we are fighting an ongoing battle of cellular aging. Osteopenia and osteoporosis occurs because of excessive oxidative stress, lack of exercise, loss of muscle mass, hormone decline, digestive issues, poor circulation and chronic inflammation. In order to prevent osteoporosis, your body needs to become more anabolic, building your muscles and bone health through a nutrient-rich diet, weight and resistant exercise, maintaining your hormones, and supporting nutrient deficiencies.
Build Muscle with Protein
One of the primary ways to improve the health of your bones is to properly feed the muscles that hold our skeletal structure. Consuming 1.2 – 1.5 grams of lean protein per kilogram of your body weight will help you build muscle mass. I generally encourage most patients, with the exception of those with kidney disease, to consume 20-30 grams of protein at every meal. Protein can help increase levels of IGF-1, an important growth hormone, and provide amino acids crucial for collagen. Healthy protein sources include grassfed beef, eggs, chicken, fish, nuts, legumes, quinoa, whey and hemp powder.
In addition to adequate protein, a diet high in fruits and vegetables promotes a good acid-alkaline balance. Avoid foods with refined sugar and limit alcohol consumption. If you feel inflamed in your body consider avoiding the nightshade foods including tomatoes, eggplant, peppers and potatoes. Limit processed foods and monitor your daily sodium intake as too much salt, especially from processed foods, can increase your calcium loss through the urine.
Important Nutrients for Optimal Bone Health
Calcium is an important nutrient for the mineralization of bone. It is important for blood clotting, nerve health, muscle contractions and other enzyme activities in the body. Eating calcium-rich foods is the preferred method to maintain adequate calcium levels in the body. The best dietary sources of calcium include dairy products, figs, kale, broccoli, bok choy, mustard greens, turnip greens, sea vegetables, bean sprouts, spinach, teff, nuts, seeds, beans and tofu.
Calcium supplementation has been shown to reduce bone loss during menopause. In general, there is conflicting research about the benefits of calcium supplements for reducing fracture risk. In recent years, several studies have linked calcium supplements to increased cardiovascular risk, colon polyps and kidney stones. New research is emerging linking benefits to a unique form of calcium supplement called Antiorbital Ionic Calcium. This form has shown benefits in osteoporosis, mitochondrial function, and lowered oxidative stress in several case reports.
Magnesium is one of the most important minerals in the body. Low magnesium levels can decrease new bone formation and increase bone resorption. Magnesium plays a role in the production of calcitonin and parathyroid hormone, which are necessary for bone health. It also plays a role in supporting cellular energy, nerve health, cell membrane health, electrolyte balance and it is involved in over 300 enzymatic reactions in the body.
The best dietary sources of magnesium are legumes, whole grains, broccoli, green leafy vegetables, animal proteins, seeds, nuts and chocolate. The best forms of magnesium to take are magnesium glycinate, citrate, ascorbate, aspartate, gluconate or malate. Magnesium oxide is not very absorbable so it is not great for bone health but it is appropriate for constipation. Optimal magnesium dosage is 400 – 600 mg per day, but some people may experience loose stools with magnesium and will need to take less. The ratio of calcium to magnesium supplement dosage should be approximately 2:1.
Zinc deficiency contributes to increased bone loss and low bone mineral density. Low zinc levels are seen with malabsorption, alcoholism and longer-duration, intense exercise. Zinc is naturally found in seafood, beef, chicken, liver, spinach, nuts and seeds. If zinc levels are low on lab work, zinc supplementation of 15 – 30 mg per day is appropriate. The best zinc supplements are zinc picolinate, zinc glycinate, zinc citrate.
Potassium can help decrease urinary calcium loss and support acid-base balance in the body. Get your potassium from food sources instead of supplements. Potassium can be found in fruits, vegetables and beans.
Boron supplementation has been shown to increase bone mineral density by increasing estrogen levels in post-menopausal women. Dietary sources of boron include prunes, grapes, peanuts, pecans, apples, beans and vegetables. Boron citrate supplementation ranges from 3 to 20 mg per day.
Silica is an important trace mineral for building collagen, which is critical for maintaining bone strength. This mineral is found in grains, fruits and vegetables as well as horsetail herbal tea. Silica 6x, a cell salt supplement, is ideal for supporting collagen production and bone health in the body.
B complex formulas that include B2, B6, B12 and folate also provide important cofactors for decreasing fracture risk.
Vitamin C is one of the most important antioxidants in the body. It supports collagen formation, energy production and immune health. Dietary sources include fruits and vegetables but especially citrus fruits. Dosage of vitamin C supplementation is 1,000mg – 2,000mg per day.
Vitamin D at an optimal level will enhance the absorption of calcium, improve strength and reduce fracture risk. Optimal vitamin D levels are between 50 – 70ng/ml. Sources of vitamin D include sunlight exposure without sunscreen 5-10 minutes per day, cod liver oil, oily fish, fortified milk, fortified orange juice. Adult vitamin D supplement dosage is generally 2,000IU per day but can be higher if there is a deficiency. Vitamin D is a fat-soluble vitamin which builds up in the body. Taking too much vitamin D for long periods of time can cause kidney failure and chronic kidney disease. If you have osteoporosis your levels of vitamin D should be tested twice per year to optimize levels.
Vitamin K deficiency can cause low bone mineral density and increased fracture risk. Vitamin D increases calcium absorption in the gut while vitamin K decreases calcium loss in the urine. Vitamin K is found in asparagus, kale, broccoli, spinach, seaweed, meat, liver and milk. This vitamin helps with bone formation. For osteoporosis, 1mg per day of supplemental vitamin K is recommended. The MK-7 form of vitamin K is more effective than other forms.
Amino acids are the building blocks of proteins which are critical for bone health. These acids play a role in the growth and repair of all tissues, including bone collagen. Lysine is one of the amino acids that is important for bone health. Lysine can be found in meat, dairy and eggs. Vegetarians with osteoporosis should supplement with 500mg per day of l-lysine. Amino acids can be found in eggs, dairy, soy, meat and legumes.
Build Strength and Agility with Exercise
The optimal time for building bone strength is during adolescence and young adulthood. That said, you can still build bone into your 60’s and 70’s through exercise. Pairing aerobic exercise at least 2-3 times per week for 20-30 minutes with high-intensity resistance and impact training (HiRIT) at least 2-3 times per week for 20-30 minutes is ideal for improving bone strength. Be aware that you also need to incorporate exercises that strengthen your coordination and your agility to help prevent falls. Contrary to popular belief, walking by itself is not enough to build muscle and maintain strong bones. However, walking while wearing a weighted vest is beneficial for improving bone strength and preventing osteoporosis.
If you are overwhelmed by the idea of lifting weights and resistance training, check out a local recreation center or gym and ask to meet with one of the personal trainers who can help create an individualized plan. A physical therapist or a certified strength and conditioning trainer can help get you started and reduce your risk of injury.
Check out Part 1 of our bone health newsletters if you missed it!
Sources:
The Whole Body Approach to Osteoporosis. R. Keith McCormick, DC. 2008.
Great Bones: Taking Control of Your Osteoporosis. R. Keith McCormick, DC. 2023.
Prescription for Natural Cures. James F. Balch, MD. Mark Stengler, N.M.D. 2016.
AANP Presentation: They’re not just in your bones: Roles of calcitonin and osteocalcin in systemic ionic calcium balance and signaling.Ryan Bradley, ND, MPH. July 2024.